Celiac Disease 101 – A Beginner’s Guide to Healing
Celiac disease has many unspoken horrible truths…
One of them is this: It takes on average 4 years to get a Celiac disease diagnosis, and the research often shows that over 2 years later most patients are still not healed and typically suffering, even though they’re eating a strict gluten-free diet. This article is an attempt to change that, to give you your power back and actually help you get back to a healthy life.
This guide was written for you, the diagnosed Celiac disease sufferer, to explain what’s happening in your body, what this means for your future, and how you can heal from this disease.
It’s intended to fill in the gaps your doctor likely didn’t tell you (and beware… there’s so many it’s almost criminal).
I wrote this because Jordan Reasoner, my best friend, had to fight for 3 years to get a diagnosis, and afterwards all he received was a small package telling him to eat a gluten-free diet and he’d be okay.
But he wasn’t…
Two years after following the gluten-free diet with cult-like strictness… he was even closer to dying. It wasn’t working and the doctors threw up their hands and said:
“You’re obviously cheating on the diet and we can’t help you any more.”
Sadly, this is now the norm in our current medical system – undereducated and under-resourced doctors blaming and misinforming patients about what it actually takes to heal from Celiac disease and what the risks of this disease mean for your life.
But it doesn’t have to be this way.
Jordan’s healed and happy now, and we’ve since helped thousands of other Celiac disease victims who’ve gone through the same struggle – and helped them recover their health just like him.
But I’m still pissed off, so I’m writing this…
My goal is to help you avoid ongoing pain – to understand your health risks – and to learn how to return to a normal healthy life if you choose.
Spoiler Alert! Another horrible truth most people with Celiac disease discover too late: the gluten-free diet on its own isn’t enough to heal — more specifics on this later.
How to Use This Comprehensive Celiac Disease Guide
This guide is all-inclusive, which means this will take you about 15 minutes to read. And since I don’t know how educated you are, we’ve put together a table of contents so you can skip to the most important parts for you:
What is Celiac Disease?
Signs, Symptoms and Prevalence
The Dangerous Risks of Untreated Celiac
Celiac Disease vs. Gluten Intolerance
From Gluten Senstive to Full-Blown Celiac
Simplifying the Toxicity of Gluten
Testing for Celiac and Gluten Intolerance
4 Tests for Celiac and Gluten Intolerance
Conventional Celiac Treatment
3 Epic Failures of Conventional Treatment
How Autoimmune Disease Develops
4 Steps for Root-Cause Healing
Conclusion
I hope you’ll leave a comment or share this with others – it’s our hope that we can save the lives of many with this article.
What is Celiac Disease?

Celiac disease is an autoimmune disease that causes damage to the small intestine, which leads to systemic inflammation, nutrient malabsorption and many other significant health issues. An autoimmune condition is a condition in which your immune system gets confused and, instead of fighting off foreign invaders, it begins to attack you.
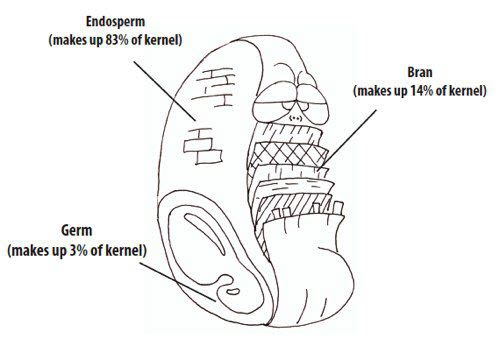
The part of the small intestine that gets most damaged is usually the villi. These are little shag carpet-like projections inside the small intestine and are vital to our health. They increase the surface area of the small intestine, give off digestive enzymes and help collect and absorb nutrients.
During the progression of Celiac disease, the villi go from vital strands to flattened and broken. This is bad news for our health.
Since it’s an autoimmune disease, that means there’s a trigger or environmental reason that creates the inflammation, immune dysregulation and subsequent problems.
The environmental trigger for Celiac disease is thought to be only gluten, which is why there’s such a focus on gluten-free foods. But, sadly, this focus on only gluten is harming most Celiacs and, in my opinion, actually killing some of them. More on this later.
Signs, Symptoms and Prevalence of Celiac Disease
Another horrible truth of Celiac disease is that while the damage does happen in the gut, only 40% of children and 60% of adults report any digestion-related symptoms.
This is one of the more frustrating parts of Celiac disease – it can cause problems all over our body. This is thought to be one of the reasons why the vast majority of Celiac disease sufferers (83% – 97%) remain undiagnosed.
Most people have multiple issues from the list below — how many do you have?
Common Signs and Symptoms of Celiac Disease:
- Diarrhea
- Gas
- Bloating and Cramping
- Constipation
- Stomach Pain
- Nausea and Vomiting
- Anemia
- Fatigue
- Joint and Bone Pain (arthritis)
- Skin Rashes
- Headaches and Migraines
- Numb Hands and Feet
- Depression
- Anxiety
- Canker Sores
- Unexplained Weight Loss or Gain
- Malnutrition
- Brain Fog
- ADHD
- Acid Reflux (GERD)
- Teeth and Gum Problems
What’s really sad about this list is the number of people who are suffering. A 2012 research study estimates about 0.71% of Americans have Celiac disease (3 Million total), meaning if you or someone in your family doesn’t have Celiac someone you know does.
Most experts now believe that number is closer to 1%, which is roughly the same prevalence found around the world, including Europe and Italy.
The risks of having Celiac disease don’t just stop with the symptom list above. Remember, a large percentage (up to 60%) don’t perceive they’re sick, which is scary when you look at how Celiac disease sets you up for lots of other health issues.
The Dangerous Risks Of Untreated Celiac Disease
Often, there’s some major denial when being diagnosed with a serious disease like Celiac. And that’s totally normal, but I want to encourage you to not wait too long to take serious action towards healing.
Because if you do ignore, deny, or fail to check your healing progress, you will most likely end up among one (or many) of these scary statistics:
- Other autoimmune disorders: Celiacs are 8+ times more likely to develop another autoimmune disease.
- Developing Osteoporosis:Celiac disease is 17 times more prevalent among the osteoporotic population.
- Having infertility issues: Celiac disease is 2.86 times more common in infertile women.
- Experiencing neurological conditions: Patients with CD are 2.58 times more prone to be stricken with neurological disorders.
- Cancer Risk: Celiac patients have a 2.44x increased risk of developing all cancers (and it rises the older you are) but GI cancer risk is much higher!
- 30% increased risk for Gastrointestinal cancer
- 40X increased risk for non-Hodgkin’s lymphoma of the small intestine
- 77X increased risk for lymphoma
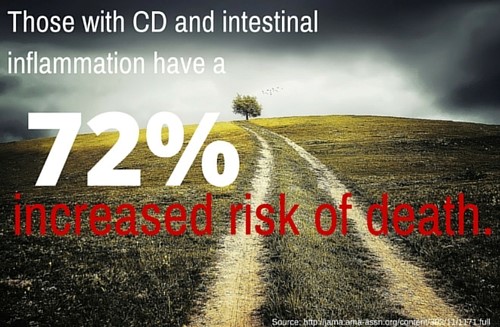
- Death Risk: Celiac patients’ risk of mortality rises extremely fast, even if you are “asymptomatic” (meaning you don’t feel it). For those with full villous atrophy, there’s a 2.88x increased risk of death in the first year after diagnosis. And those with intestinal inflammation but not full villous atrophy had a 4.66x increased risk of death in the first year.
In other words, if you’re a symptom-free Celiac and your labs show signs of gut inflammation… you’re still at significant risk of health complications and early death.
Look, I’m not trying to scare you, I just want you to be a fully-informed patient – the kind of patient that can make the best choices for their bodies and lives, not one whose power is in the hands of a doctor (who frankly doesn’t have the time and attention to have that kind of power to begin with).
And it all starts by facing the (sometimes brutal) realities of life.
But don’t worry… the above scenarios don’t have to become your reality… In fact, I’m giving you the steps to avoid joining those statistics (like MOST Celiacs), and instead properly heal.
The Difference Between Celiac Disease & Gluten Intolerance
It’s not like you just woke up one day and suddenly “caught” Celiac disease. Instead, you’ve been progressively getting sicker and the amount of damage inside your body has been slowly building…
Which is the core difference between you and those who are suffering from gluten intolerance, or what’s also called Non-Celiac Gluten Sensitivity (NCGS). The University of Maryland currently reports about 18 Million Americans (6% of U.S. population) have this condition.
However, this is the lowest estimate of affected people…
Dr. Alessio Fasano, Director of the Center of Celiac Research, has repeatedly said,
“All humans lack the enzymes required to break down gluten.”
And now, new studies are coming out that propose mechanisms to support this statement, meaning the actual number of people with gluten-related problems could be well into the 100’s of Millions. It’s worth noting that just because it’s extremely hard to digest it doesn’t mean everyone has a gluten issue.
Those with gluten intolerance can experience all the same symptoms listed above for Celiacs, like diarrhea or constipation, hives, brain fog, bloating, and headaches.
Like Celiac disease, gluten sensitivity is a condition in which the immune system is activated by gluten, causing inflammation and intestinal permeability. But the immune system is not attacking the lining of the small intestine, like it is in Celiac disease.
So, the main difference between gluten intolerance and Celiac disease is in the way the immune system is reacting to gluten and gliadin. But let’s be clear, in both cases there is an immune response to wheat.
The immune response of a NCGS person is not directed at the human tissue… it’s directed at the environmental trigger.
However, leading Celiac disease experts, like Dr. Tom O’Bryan, believe that Celiac disease isn’t like a light switch… it doesn’t just turn on or off. They believe that even those with NCGS have some immune cells attacking the human tissue but at too low of a level for our current medical tests to detect.
And after months or years of this “silent” attack, the immune response begins to grow in severity until it’s finally detectable by our current laboratory tests.
With that being said, if you are gluten intolerant, the advice of this article is just as relevant for you as it is to a diagnosed Celiac disease person.
Going From Gluten Sensitive to Full-Blown Celiac Disease
Many Celiacs don’t actually get diagnosed with full-blown Celiac disease until later in their lives (20s, 30s, 40s, 50s and beyond)… which is fascinating and usually confusing when it all happens. At this point, they may wonder if they were gluten intolerant that whole time?
Let’s explore how Celiac disease develops and what role gluten intolerance plays in it — as we do remember the difference between the two is mainly in how dysregulated the immune system is.
There’s two main sides to the immune system – the innate and the adaptive. Each has a large role in keeping us healthy.
In gluten sensitivity, both are thought to actively attack gluten and other molecules that are getting into your bloodstream because of a leaky gut (more on what this is later).
In Celiac disease, the adaptive side goes haywire and begins to attack your gut cells thinking they too are foreign molecules that should be destroyed. This is the autoimmune component of the disease.
Simplifying the Toxicity of Gluten
In both gluten sensitivity and Celiac disease, the damage and discomfort is driven by gluten and avoiding it is critical for healing. But it is hard to avoid something you don’t understand. We need to know what exactly gluten is and how we can avoid it.
You probably already know this, but gluten is a protein found in barley, rye and wheat.
Here is what you probably don’t know: plants don’t want to be eaten by you. In fact, they have a complex series of defense mechanisms to prevent humans and other animals from eating them.
One of these defense mechanisms are toxic proteins, called prolamins, contained in virtually all cereal grains (gluten-free or not). And gluten happens to harbor one of the most toxic prolamins – gliadin -and it is this gliadin in gluten that causes the damage.
Gliadin even inflames the gut of healthy individuals. But for those with gluten sensitivity or a genetic predisposition to Celiac disease, the damage is far worse.
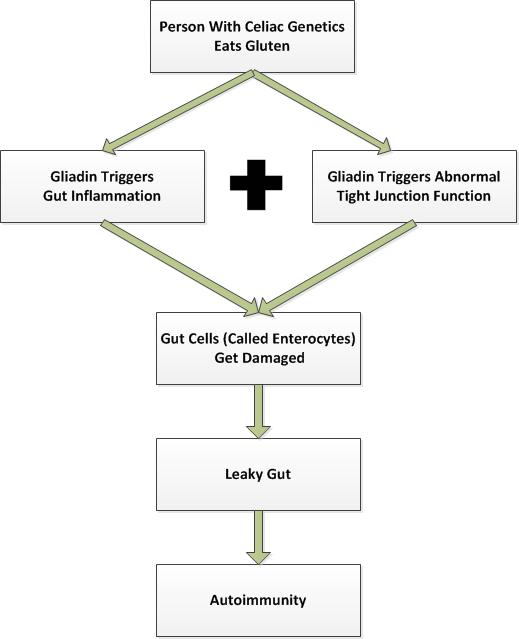
When a person with the genetics for Celiac disease eats a bagel, a bowl of pasta, or anything else containing gluten, damage occurs in a few ways:
- Gut Inflammation – The human gut (and the gut of many other animals) has a very hard time breaking down the proteins like gliadin in gluten. The immune system actually attacks the particles, which also causes damage to healthy tissue, increasing gut inflammation.
- Leaky Gut – Gliadin triggers an increase in zonulin levels, causing intestinal permeability. Zonulin is a “gatekeeper” protein in the human gut that controls the tight junctions of the gut (where nutrients pass out of the gut and into the bloodstream). When zonulin levels increase, the tight junctions open up wider and allow the larger gliadin molecules to pass into the bloodstream – and create a leaky gut.
- Autoimmune Reaction – Gliadin gets through the gut wall and begins to cross-link with an enzyme called Tissue Transglutaminase (tTG). This is a repair enzyme released to fix gut cells (enterocytes) that are damaged when ingesting gliadin. This cross-linking triggers production of antibodies that attack enterocytes, causing ongoing autoimmune destruction.
The increase in zonulin (and resulting widening of the tight junctions) leads to the development of a leaky gut.
It’s worth noting that there are actually at least 19 triggers of leaky gut – gluten is just one of them.
Free Leaky Gut Presentation: Click here to learn the 19 common triggers of leaky gut and how to heal from them.
So, in short, prolamins are defense proteins found in plants. Gluten is just one of several types of prolamins and contains a specifically toxic part called gliadin. In general, while wheat, rye and barley are thought to be the worst offenders for Celiacs, once the damage has begun, any prolamin – whether from a grain or pseudograin – can be problematic.
With that said, let’s talk about how to actually confirm you have Celiac disease.
Testing for Celiac Disease and Gluten Intolerance
There’s a lot of confusion around the testing and diagnosis of Celiac disease and for good measure, which is why, on average, it takes a Celiac 4 years to get the proper diagnosis. Frankly, this is pathetic and downright sad. I believe patients can speed up this process by being more educated than their doctors on the subject.
Technically, a Celiac disease diagnosis is determined based upon histologic demonstration with supporting criteria, meaning that there’s no one “perfect” test to diagnose the disease.
What’s going on is doctors are looking for a specific amount of damage to your small intestine and backing it up with test results to confirm you have the risk factors for the disease.
In more simple terms, that means when gluten intolerance crosses a small-intestine-damage threshold and autoimmune risk factors are confirmed via lab tests or autoimmune markers are actually observed on your lab work… then you officially have the diagnosis of Celiac disease.
4 Tests for Celiac Disease and Gluten Intolerance
Since there’s so much confusion around the testing here…
Let’s break the tests into 3 categories:
- Supportive
- Autoimmune
- Damage
1.) Supportive Tests – Typically, these are tests that that are the easiest and cheapest to run. They provide supporting evidence for risk of Celiac disease or Gluten sensitivity.
An example of a supportive test, would be getting a genetic test to check for Celiac disease genes. You can do a serum lab test or even 23andme.com testing to figure this out (meaning you don’t need to wait for your doctor to do this testing).
2.) Autoimmune Tests – These are tests used to check for and measure the level of immune system dysregulation going on in your body. There is a major drawback with these tests, though, you’ll need to have eaten gluten in the last 2-3 months to get an accurate result.
A blood test called a tTg-IgA test (Tissue Transglutaminase Test), which looks for antibodies in your blood towards gluten, is the oldest and cheapest test. However, this means there are some big drawbacks to it, including possibilities of false negatives and a positive result might mean you have something other than Celiac disease!
Bottom line for the tTg-IgA test: If you are positive or negative, it doesn’t mean you DO or DON’T have Celiac disease.
The most advanced blood test on the market, Cyrex Array 3, is the first one to check your immune reactivity to all parts of gluten, gliadin and other parts transglutaminase. This test, while still pretty new to the market, is the first of its kind to take a holistic approach in checking for wheat sensitivity. It’s currently the best option of the autoimmune tests.
3.) Damage Tests – These tests are the last step – they’re the most expensive and intrusive. However, at this time, in order to get an “official” Celiac diagnosis from a doctor, this test is the last piece of the puzzle.
It’s called an endoscopic biopsy (small intestine biopsy), and it’s where doctors actually go in and remove a part of your intestine and look at it under the microscope to check the damage. Hopefully, in the future, new testing will be developed that won’t be so invasive to the body.
In conclusion, the best approach for obtaining a proper diagnosis is to first get your genetics checked. Then, get a Cyrex Array 3. And if both are positive, get an endoscopic biopsy. If you get a positive test result from the endoscopy, it’s a big red flag you’ve had this condition for a long time and you’re likely going to need to take your healing process very seriously.
Feeling better after gluten removal isn’t enough to be diagnosed as Celiac, but it’s a really good sign that you’re AT LEAST gluten intolerant. And based on the several Cyrex Array 3 tests I’ve seen, you’d turn up plenty of positives there.
Conventional Celiac Disease Treatment
After you finally get your diagnosis, which will typically take you 4 years or longer, your conventional medical doctor will probably tell you this…
“Adopting a strict gluten-free diet is the only known treatment for those with gluten-related disorders.” – From the Celiac Disease Foundation
At first, just making this change seems so hard and sometimes impossible, especially giving up those treasured foods you may have grown up with. But the majority of Celiacs I’ve talked to finally make the change and begin to live the gluten-free lifestyle.
And they end up loving this new lifestyle because they feel so much better than before.
But most end up hitting a glass ceiling of healing. In other words, their really painful symptoms might decrease or mostly go away but they don’t get the energy, skin, hair, weight regulation and dependable brain and digestion they are really wanting.
And it’s NOT their fault or your fault.
You’re being told to follow a treatment that has abysmal results in actually healing Celiac disease.
I know, this is hard to believe but I’ll prove it with scientific studies in the next section.
3 Epic Failures of Conventional Celiac Treatment
After 2 years on the gluten-free diet, your chances of fully healing your intestines are between 8% and 34%.
2 years of effort for way worse than a coin’s flip chance at healing!
But it only gets worse…
The intestinal leakiness of Celiacs who’d been off gluten for 2 years was found to be 3x more leaky than controls.
WAIT! You might think, “What about those who get symptom-free on a gluten-free diet? Doesn’t that mean all is okay?”
No.
This study and this study looked at inflammation levels in “symptom-free” Celiacs and found significant amounts of inflammation, compared to control subjects.
And it gets even worse, 18 of 30 Celiacs who had been gluten free for 8-12 years, with biopsy-proven health, had poor vitamin status (malnourishment).
In other words, the gluten-free diet can help you get symptom-free, even repair your villi (proven by biopsy), but it’s unlikely you’ll also repair leaky gut syndrome, reduce inflammation to normal amounts and replace lost nutrients from the malabsorption the disease causes.
It’s time to treat Celiac holistically and use strategies to address the known issues. Yes, you need to avoid the environmental trigger (gluten). But it’s clear that if that’s all you do… well, remember those scary associated conditions like brain, fertility and cancer?
…the Gluten free diet leaves you vulnerable to all of them.
How Autoimmune Disease Develops (and Why This Gives You Hope)
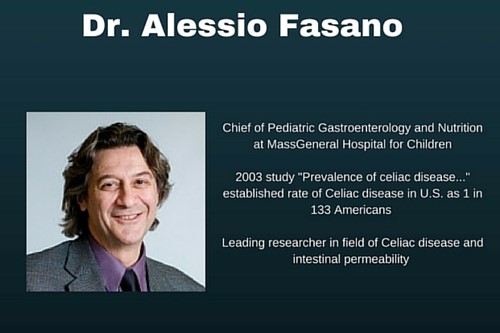
In 2011, Celiac researcher and doctor, Alessio Fasano released his groundbreaking paper, “Leaky Gut and Autoimmune Diseases.” Fasano proposed that this autoimmune attack could actually be stopped!
This is really good news… because, up until this point, it was assumed that once the autoimmune process starts, it’s just going to continue attacking your body for the rest of your life.
But Fasano’s latest research, conducted over several years, has shown that it is indeed possible to stop the attack on the body’s own tissues and usually repair the damage that has happened (if it’s not too beat up).
Fasano’s Theory of Autoimmunity Development Requires 3 Factors:
- A genetic predisposition to autoimmunity (for Celiac disease that’s the HLA DQ2/DQ8 genes)
- Exposure to an environmental trigger (for Celiac disease – gluten)
- Increased intestinal permeability (a.k.a. Leaky Gut Syndrome)
According to Fasano, when all three of these factors are simultaneously present, autoimmunity develops. This means if you have Celiac or another autoimmune condition, you had to have a leaky gut at the time it started (and it’s likely you still might).
So, this theory finally explains how you could have the genetics for Celiac disease yet remained mostly healthy your whole life. And then BAM! You have a mid-life crisis at 46 that triggers leaky gut, you’re eating gluten and “all of a sudden”you have a full-blown autoimmune disease.
However, there is a silver lining to all of this!
If having a leaky gut is the final factor that allows autoimmune disease to develop, then autoimmune disease can be stopped and most people can heal the damage by fixing the intestinal permeability and removing the trigger (gluten).
This is a whole new way of thinking about Autoimmune disease – one that gives us the steps needed to actually heal the body, instead of becoming another untreated Celiac disease statistic.
It’s also why we now know that while removing gluten (the trigger) is the most important step… it’s not nearly enough to heal a leaky gut and stop the autoimmunity completely. There’s more work to be done before the process has been fully arrested.
Now can you see why the gluten-free diet as the “only treatment” for Celiac disease is just silly?
4 Steps for Root-Cause Healing of Celiac Disease
Here are the 4 steps you need to focus on to actually heal the destruction from Celiac disease. This plan actually takes into account all four of the problems shown in the research to be plaguing Celiac suffers.
This is the plan to heal a leaky gut and reverse the damage from years of untreated Celiac disease…
And it starts with removing gluten from your life. This is still a must!
Step 1 – Remove Gluten (from all food, products, etc.)
It’s time to throw away all the packaged or processed foods in your kitchen that don’t have a gluten-free label on them. There’s no reason to keep any old flour or foods, period. Don’t leave any room for temptation.
You also need to read the labels on any product you put on your skin – shampoo, moisturizer, lotion, chapstick, etc. Ideally, it’s best to think of your skin as a giant extension of your tongue and don’t put anything on it you wouldn’t eat! So, verify that all these products are gluten-free as well.
Next, take a close look at your kitchen hygiene. If there are gluten eaters in the house, you cannot use their non-stick pans (don’t use them, they are toxic), cutting boards, or kitchen utensils. It’s even best to avoid using the same counters. Yes, that is kind of dramatic feeling. But the truth is even trace amounts of gluten can harm you. And if you can’t be safe at home, where you are in control, where can you be?
When you do eat out, don’t be shy about letting your server know of the severity of your condition. To be fully prepared, it’s best to call ahead and verify they can guarantee no cross-contamination. If they can’t guarantee it, there’s a good chance that sooner or later they will serve you some gluten. Here’s a guide to help you eat out gluten-free.
Step 2 – Add Nutritious Foods
It’s clear, from the research, that you need more nutrients than most people and you need to do everything in your power to reduce inflammation.
And this means it’s time to add in some highly-nutritious foods to help replenish the nutrient depletions in your body and give it what it needs to heal. (It costs a lot of nutrients to heal!)
At the same time, these foods will be extremely anti-inflammatory.
It’s a double-whammy move to help you heal.
This means you’ll need to eat A LOT more meat and seafood. It means eating more vegetables, fruits, and naturally starchy foods (sweet potato, white potato, white rice, etc). It means eating more healthy fats, like avocado and coconut products.
And it means eliminating all grains and pseudograins (even “gluten-free” grains, like corn and oats). Why? Because these foods have their own “gluten-like” prolamins that wreak havoc in inflamed and damaged guts.
In order to make room for all these new unprocessed and delicious foods, you’ll be eating very little processed gluten-free foods, which will actually save you a bunch of money.
In our experience, the stricter you are to adhering to these rules, the faster you’re likely to heal and feel better.
Step 3 – Heal the Leaky Gut
While cutting out gluten is a pretty straightforward proposal, healing a leaky gut is more complex.
There are endless free tips online on how to heal your leaky gut (some of them are good but many are actually pretty bad), which is why we hired 3 researchers to look at the most current studies and help us figure out the best way to actually do it.
Then, we took these protocols and put them into practice and have seen nothing short of amazing results in 1000’s of people.
One of the first steps to heal a leaky gut is to avoid grains and pseudograins, the ones I told you about in the previous section. Eating the diet above is ideal for healing it.
Next up, you’ll want to try some proven gut-healing supplements, like L-Glutamine. It’s been shown to heal your intestinal mucosa and reduce leaky gut. Start at 2.5 g morning and evening and work up to 20 g morning and night, over two weeks. (Read our complete recommendations on L-Glutamine Do’s and Don’ts.)
With that said, there are 19 triggers of leaky gut and many other helpful supplements out there.
Step 4 – Improve Inflammatory Lifestyles
The last step is used to reduce your inflammation and heal your leaky gut. And it’s all about your lifestyle.
Many Celiacs are unknowingly choosing a lifestyle that creates disease. This includes doing things like going to the gym every day, training for and running marathons, CrossFitting 5 times a week, sleeping less than 7 hours a day, using caffeine after noon, and drinking excess alcohol each night.
Each of these behaviors creates more inflammation and contributes to leaky gut syndrome.
No, don’t freak out! I still want you to work out and exercise, just less strenuously until you’re in better health. I don’t believe that coffee is really bad, but it surely is after noon because it messes up sleep cycles. And I don’t think wine or alcohol is necessarily toxic, but drinking more than one day a week is definitely hurting your gut.
Look, you’re changing your diet, you’re healing your leaky gut, it’s time to take this seriously and that includes cutting out lifestyle habits that are harming you.
In Conclusion…
Okay, so if you made it this far, you’ll likely be better educated than your doctor on your disease (which is impressive).
Let’s review the important take-home points:
- Celiac disease is an autoimmune disease where the body attacks the lining of the small intestine
- Celiac disease and all other autoimmune diseases occur when 3 conditions are met
- Genetic predisposition
- Environmental trigger
- Leaky gut
- Gliadin (a protein in gluten) causes an increase in zonulin, which controls the widening of tight junctions in the gut, creating a leaky gut in those with Celiac who eat gluten
- If you don’t heal your digestive tract, your risk for most disease and early death rise dramatically
- The gluten-free diet alone isn’t enough to heal you
- There are four steps to treating Celiac disease based on the research
- Avoid gluten in food and in all products you put on your skin
- Eat a more nutritious diet to replace malabsorption caused by disease
- Heal your leaky gut
- Change your lifestyle to help you avoid leaky gut and inflammation
You are now armed with the basic information to really handle and overcome Celiac disease. I hope you share this with others you know who are affected. And let us know in the comments what your number one takeaway from this article is.
Steve
Note: We earn a small commission, if you use the product links on this page to purchase the products we mention. We only recommend products we would use or have used in the past. Your purchase helps support our site and ongoing research.
Did You Like this Article?
Subscribe to our newsletter to receive email notifications, some ways to find relief, and next steps.